I have seriously committed to doing what it takes to feel better while living with borderline personality disorder (BPD). For years, I’ve attended weekly therapy, seen my psychiatrist monthly, followed my medication plan closely, focused on a healthy diet, exercised regularly, and intentionally strengthened my support network.
In many ways, I’m thriving. Truly.
Which is exactly why it’s so frustrating that “BPD days” still show up.
They’re still here. They probably always will be. All these tools and resources don’t erase them—they just make them slightly easier to cope with. And honestly? Some days they still don’t feel very “bearable” at all.
Understanding BPD Triggers and Anxiety Responses
Therapy has helped me identify many of my BPD triggers. I can recognize when my thoughts aren’t aligned with reality—but knowing that doesn’t stop the physical symptoms.
Anxiety has always been my Achilles’ heel.
After more than a decade of therapy, I’ve finally been able to understand anxiety for what it is: a coping mechanism my brain developed to protect me. And it makes sense. As a child who experienced sexual abuse and emotional neglect, being hyper-vigilant—being “ready for anything”—kept me safe.
The problem is that this pattern didn’t stop when the danger did.
My nervous system still defaults to fight, freeze, or flight, even when I’m surrounded by safety, support, and healthy relationships.
For years, as I worked on empowerment and autonomy , I shifted from one side to the other, from freezing to fighting. At first, it felt powerful. I felt less helpless.
But eventually, it turned into defensiveness and aggression—and that didn’t work either.
Searching for the “Middle Ground” With BPD
Finding the midpoint—that mythical balance—has felt like searching for the Holy Grail.
Where is it?! I need it desperately.
I’ve improved in so many ways:
- I see my professional worth
- I set healthier boundaries with family and friends
- I know I need time before reacting emotionally
- I have created contingency plans with professionals to prevent psychotic episodes and suicidal ideation
Honestly, I do more emotional regulation work than many neurotypical people. (Sorry not sorry—but watching “the norm” lack self-awareness while we’re forced to develop it out of necessity can be infuriating). A bad day for neurodiverse people is not about “calming down”, it’s an alarm to activate a complex plan to provide emotional containment to avoid quick and dangerous escalations.
I’ve reached a place where I make choices based on long-term wellbeing, not immediate relief or external validation. And ironically, this more advanced stage of healing is incredibly hard.
When Deeper Trauma Surfaces
Like leveling up in a video game, the higher you go, the bigger the challenges become.
Now I’m facing the core wounds:
- Sexual abuse
- The night my mother died
- Deep feelings of unworthiness, defenselessness, anger, and guilt
These are the emotions I’d rather avoid—but they demand attention.
So I keep showing up to therapy.
The sessions that challenge me to sit with guilt instead of running from it.
The ones that ask me to recognize patterns that once kept me safe—but no longer serve me.
I no longer need to distrust everyone.
I don’t need to be aggressive to prove my worth.
I can experience disappointment and loss differently than I did as a child.
My brain understands this.
My emotions… not so much.
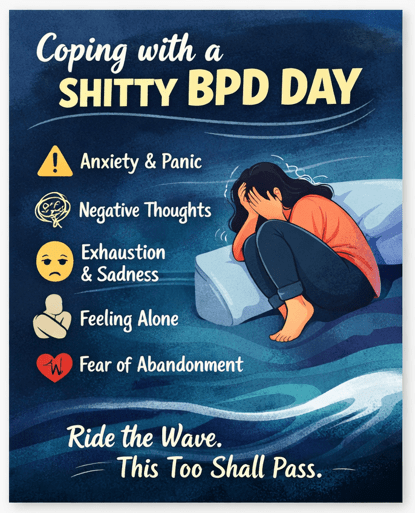
Having a Shitty BPD Day
So here it is: I am having a shitty BPD day.
They happen less often now.
They’re less intense.
But they’re still deeply uncomfortable.
Anxiety shows up as:
- Nightmares and insominia
- Sweating, a racing heart, headaches
- Nausea and vomit
- Blurred vision
- Shaking hands and general body pain
- A crushing sense of helplessness and fear
Today I didn’t leave my house. I didn’t work out. I didn’t shower. I didn’t make my bed. I barely ate. I couldn’t do the things I know help.
Instead, my inner critic took over:
- You’re not enough
- You’re alone
- You’re too much
- No one will ever truly love you
It’s exhausting. Annoying. Sad. Infuriating.
But I’ve learned something important: I don’t fight my mind on days like this anymore.
I let it rant.
I let the discomfort exist.
I remind myself it’s temporary.
In a strange way, this chaos is my brain’s outdated attempt to protect me. It just hasn’t updated the software yet.
Grief, Attachment, and Fear of Abandonment
I can trace today’s main trigger.
My dog, Pablo—my safest place—is very old. I know the goodbye is coming.
That’s not something I can control.
This taps directly into my fear of abandonment, my deep attachment, and how much I built my life around the unconditional love he’s given me.
There was a time I believed I wouldn’t survive his death.
Now, I know I owe him having a rich and peaceful life, even when he is no longer by my side—right until the end.
I’m still terrified. But now I see how he’s been teaching me to ride without training wheels all along.

Choosing Not to Fight It
Today, I let my body shake.
I cry.
I feel nauseous.
I sit with it.
But I don’t react.
I don’t send angry messages (I did delete a few chats—imperfect, but okay).
I limit alcohol.
I don’t self-destruct.
I choose self-compassion, even when I can’t do it perfectly.
I reach out to my friends.
Letting myself feel this discomfort—without running, numbing, or harming myself—feels like real progress.
A Reminder for Anyone Struggling Today
If you’re having a shitty mental health day:
- Follow your action plan (or create one)
- Reach out to your support system
- Contact your therapist or psychiatrist if needed
But most importantly: trust yourself.
This feeling is temporary.
It’s your mind’s old way of trying to keep you safe.
Today Is Hard—But It’s Only Today
I’m having a shitty BPD day.
And for once, I know they’ll keep coming—but fighting them only makes it worse.
Today, I let it be.
And today, that’s enough.
For some of us, having a clear plan can help us feel safer during those moments. This checklist was created based on the lived experiences of navigating crises with BPD. We are not mental health professionals, but we hope these tools can be supportive and relatable.
Your well‑being always comes first. If you feel at risk or unsafe, please reach out to a mental health professional or emergency service.
This document is editable—adapt it to your needs, print it, or share it.
It’s free, no emails needed.
